Stakeholders Pick Rx Costs & Pricing as Topic With Greatest Impact This Year
Clive Riddle. February 25, 2019
MCOL and Healthcare Web Summit jointly sponsored a survey of healthcare professionals on which of three key topics would have the greatest impact, and what stakeholders would be economic winners and losers during this year. Here’s a summary of the findings:
Participants were asked to respond to three items:
1. Which one of these three topics will have the greatest impact on stakeholders in 2019?
- Medicaid Funding and Eligibility
- Pharmaceutical Costs and Pricing
- Value Based Care Initiatives
2. Please project who you think the economic winners and losers for 2019 will be. Who do you think will be economically better off, the same or worse off by this time next year: Consumers; Employers; Health Plans; Hospitals; Physicians; Pharmaceutical
3. Please indicate your perspective
- Purchaser (Health Plan, Employer, TPA, Agent, PBM)
- Provider (Hospital, Physician, Pharmaceutical, Other Providers)
- Vendor or Other
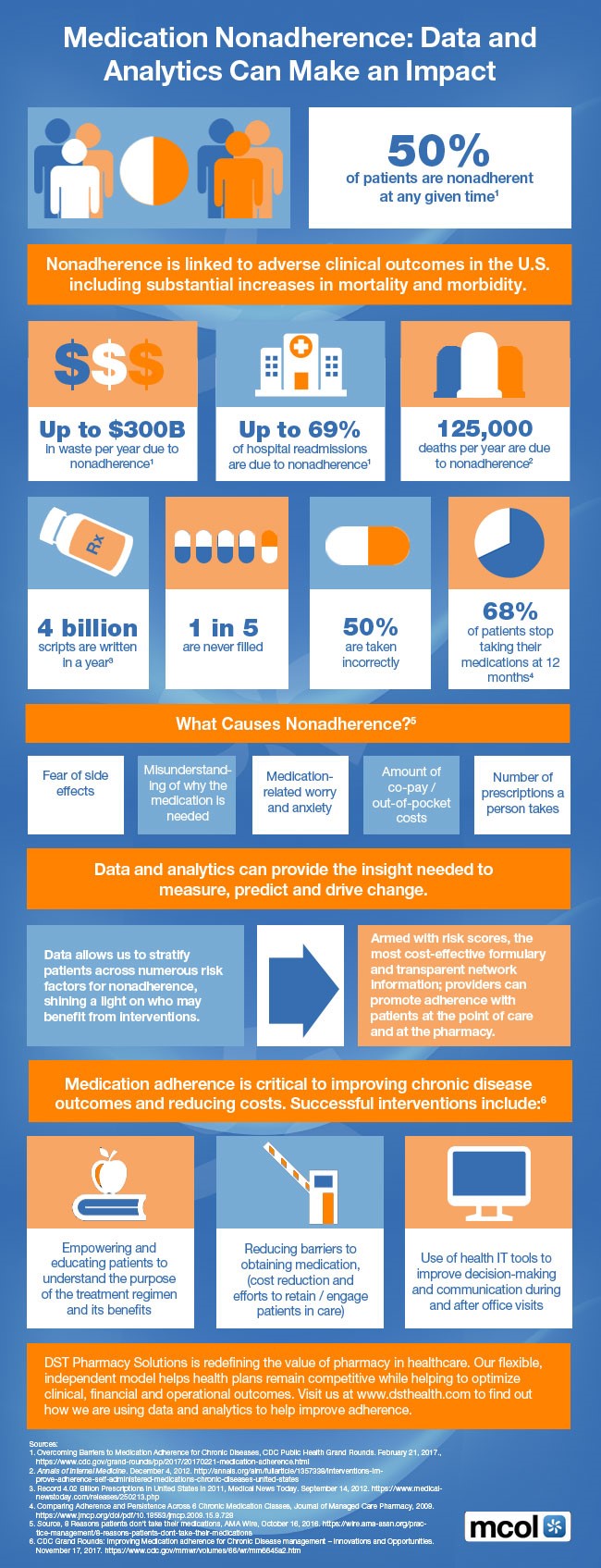
Stakeholders overall (51.7%) selected Pharmaceutical Costs and Pricing as the topic having the greatest impact in 2019, compared to Value Based Care Initiatives (31.7%) and Medicaid Funding and Eligibility (16.7%).
Providers (54.5% and Vendor/Other (52.0%) respondents both selected Rx as the top choice, but Purchasers selected Value Based Care (53.8%) slightly over Rx (46.2%). More Providers selected Medicaid (27.3%) over Value Based care (27.3%), while Vendors chose Value Based Care (32.0%) over Medicaid (16.0%)
More respondents (45.2%) overall selected Pharmaceutical Stakeholders vs. other categories as being better off in 2019 Health Plans came in second for being better off at 33.9%. Hospitals reflected the least optimism, with just 18.0% viewing them as better off this year.
Hospitals thus were viewed with the most pessimistic outlook, with 65.2% feeling they will be worse off this year. Physicians were next in line, at 56.5%.Health Plans and Pharmaceutical stakeholders tied for the least pessimism, each with 21.7% viewing them as worse off this year.
It should be noted that these levels of pessimism have generally declined from last year. The top three choices for being worse off in last year’s epoll all dropped: Consumers from 68.&% in 2018 to 38.7% in 2019; Hospitals from 57.2% in 2018 to 49.2% in 2019; and Physicians from 50.8% in 2018 to 29.0% in 2019.
Purchasers had a rosier view for Consumers and Pharmaceutical stakeholders, with 46.2% saying Consumers would be better off, compared to 23.7% of Providers and 23.1% of Vendors/Others; and 61.5% of Purchasers saying Pharmaceutical would be better off compared to 39.1% of providers and 42.3% of Vendors/Others.
Providers saw themselves in a worse position for 2019 compared to other respondents. 65.2% of Providers said Hospitals would be worse off, compared to 38.5% of Purchasers and40.0% of Vendors/Others. 56.5% of Providers said Physicians would be worse off, compared to 30.8% of Purchasers and 34.0% of Vendors/Others.

 Share This Post
Share This Post